Credentialing is one of the most important parts of providing care and medical billing. It influences the efficiency and legitimacy of healthcare service payments as well as established trust between patients and healthcare providers.
Credentialing is the process of verifying a doctor’s:
- Experience
- Training
- Schooling
- License
- Residency
- Certificate
- And other necessary experience
Credentialing in Medical Billing
To ensure healthcare providers have the proper licensing, certifications, and skills to provide proper patient care, medical organizations, and insurance companies verify their credentials. It is a comprehensive examination of a provider’s credentials, including education, training, residency, licensure, and any certifications. Credentialing guarantees that suppliers meet all of the standards established by the insurance sector and regulatory organizations. This is a mandatory process for usage with insurance providers, Medicaid, and other programs.
How Medical Billing and Credentialing Interact
Medical billing and credentialing have a synergistic relationship. Healthcare providers who lack proper credentialing may be unable to bill an insurance company for their services, resulting in delayed or denied claims. This has an influence not just on healthcare providers’ revenue cycles, but also on patients’ access to critical medical care.
Key Players
Healthcare Providers: Doctors, nurses, and other medical practitioners seeking to be credentialed.
Insurance Companies: Entities that require credentialing for providers to join their network.
Credentialing Committees: Groups within insurance companies or third-party organizations that review and approve credentialing applications.
Why Credentialing is Essential in Healthcare
Ensuring Quality and Compliance
Credentialing is critical for sustaining good standards in healthcare. It assures that only qualified and competent caregivers deliver care, protecting patient safety and well-being. It also aids in compliance with legal and regulatory regulations, reducing the risk of medical errors and misconduct.
Legal and Financial Implications
Credentialing is essential in combating healthcare fraud. It assures that only authentic and certified professionals are reimbursed for medical services by thoroughly verifying providers. This process is critical for the healthcare system’s integrity, both financially and legally.
Impact on Patient Care and Insurance Reimbursements
Proper credentialing has a direct impact on patient care by ensuring that they are treated by certified professionals. It also has an impact on the efficiency of insurance reimbursements. Credentialing providers allow claims to be processed more efficiently, decreasing payment delays and improving the overall financial health of healthcare operations.
Facilitates Trust and Credibility
When patients know that their healthcare providers are credentialed, it builds trust in the quality of care they are receiving. Being accredited by respected insurance companies improves a healthcare provider’s professional credibility and reputation.
Enhances Overall Healthcare System Efficiency
Credentialing works as a deterrent to fraudulent healthcare practices, ensuring that only legitimate providers are part of the system. By expanding the network of credentialed providers, credentialing improves patient access to a wider range of healthcare services.
Promotes Continuous Professional Development
The requirement for re-credentialing drives healthcare providers to keep their skills and knowledge up to date and in line with the most recent healthcare standards and practices.
The Credentialing Process
The credentialing process is both complex and simple. The steps are fairly straightforward, however, one snag can cost you weeks of time.
Preparing Information:
Before you submit your application for verification to the organizations listed above, you’ll want to make sure that you have copies of all information necessary for the application. Have both physical and digital copies ready to go.
Application Submission:
A medical professional begins the process by submitting an application to the healthcare facility or organization where they intend to practice. This application is thorough, demanding information about their school background, training, job history, current and previous licenses, board certifications, malpractice history, and any disciplinary actions.
Primary Source Verification:
The credentialing department ( or specialist) undertakes primary source verification after receiving the application. This stage is critical for ensuring the credibility of the credentialing process. It means contacting the institutions or organizations that granted the credentials (such as medical schools, former jobs, and licensing boards) to verify the accuracy of the applicant’s information.
Committee Review and Decision:
Once the verification is complete, a credentialing committee reviews the application and all obtained information. This committee, which is often made up of experienced healthcare professionals, hospital boards, and others, assesses the credentials against set norms and procedures. They make the choice to approve, delay, or deny the applicant’s request for privileges.
Ongoing Monitoring and Re-credentialing:
Credentialing is not a one-time event. Healthcare providers must be re-credentialed every two to three years. This procedure entails reevaluating the provider’s performance, continuing education, and any changes in their qualifications. Continuous monitoring is also carried out to verify that providers retain their standards and adhere to new recommendations or regulations.
Legal and Regulatory Considerations
Medical credentialing is heavily regulated to ensure patient safety and high-quality care. Understanding these legal and regulatory aspects is crucial:
State and Federal Regulations: Credentialing must adhere to a variety of state and federal standards. These statutes govern licensure, professional standards, and provider qualifications.
Medicare and Medicaid Requirements: To participate in Medicare and Medicaid programs, providers must be credentialed and meet their standards.
Legal Implications: Incorrect or negligent credentialing can have legal ramifications for healthcare organizations, such as malpractice lawsuits and penalties.
Ongoing Compliance: Keeping up with changing requirements and ensuring constant compliance is a key problem in the credentialing process. Consider a medical credentialing company to help you.
Challenges in the Credentialing Process
When it comes to credentialing in medical billing, it can be a complex process. There can be many hookups and challenges a medical provider can face, here are some of the most common.
Lengthy Processing Time: Creditiling processes can easily take over 90 days. So you’ll want to include this process time in your credentialing forecasting.
Paperwork Errors: Errors are the bain of any credentialing process, and yet, they still happen. Inaccuracies or incomplete information in the application can cause setbacks and require resubmission.
Changing Regulations: Keeping up with changing healthcare rules and insurance requirements can be difficult. Using a credentialing service can help keep you up to date and speed this process along.
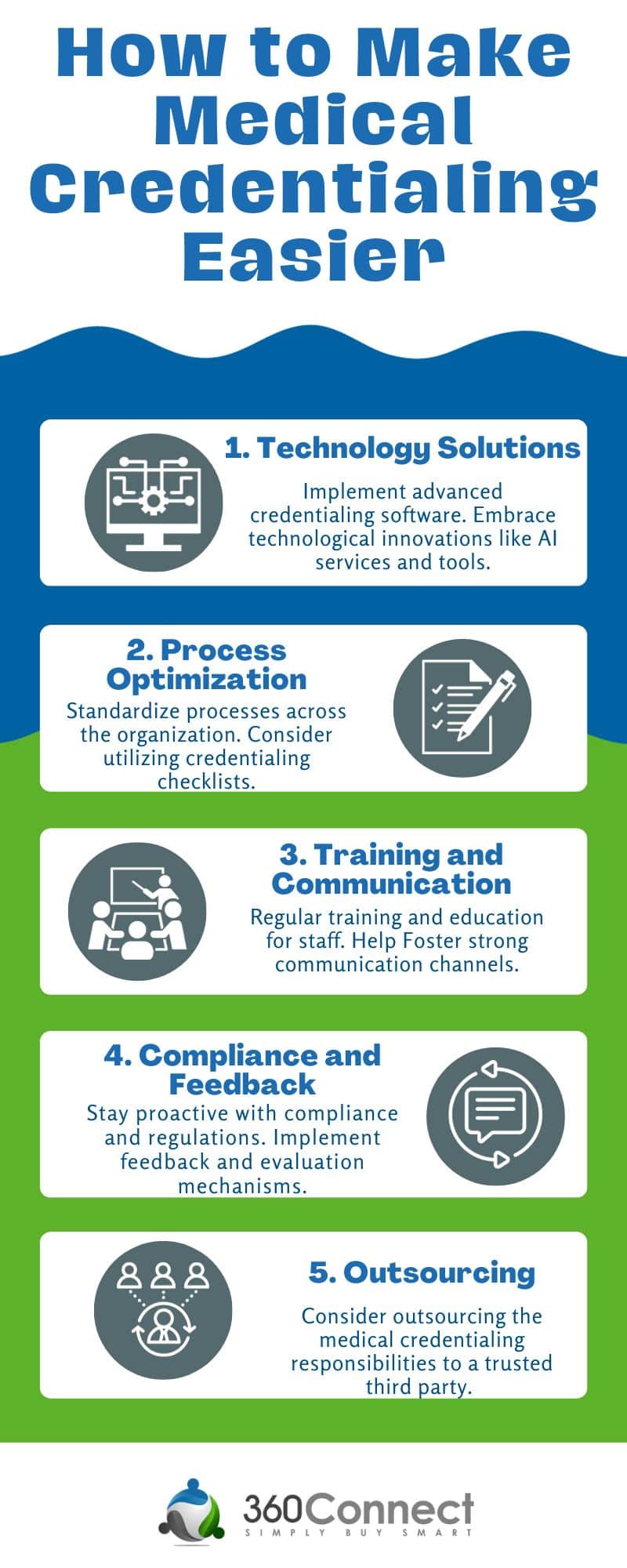
Best Practices for Efficient Credentialing
Credentialing can be a pain, but that doesn’t mean you can’t do anything to make the situation easier. There are a couple of useful tips you can use.
Early and Thorough Application Submission: Start the process well in advance and ensure all documentation is accurate and complete.
Utilize Technology: Track application status and maintain up-to-date records using credentialing software.
Regular Updates: Make sure all professional documents are up-to-date, such as licenses and certifications.
Stay Informed: Keep informed of changes in healthcare regulations and insurance policies.
Use a Medical Credentialing Service: Using a medical credentialing service can help you speed up the process and make sure you are in compliance with the law.
Types of Credentialing in Medical Billing
Initial Credentialing
- A healthcare provider’s initial credentialing occurs when he or she first applies to join a healthcare organization, network, or insurance panel.
- During this process, the provider’s qualifications are verified in detail, including their education, their training, their licensing, their work experience, and any certifications or specializations they hold.
- Typically, this process includes background checks, verification of educational credentials, and a review of malpractice history or disciplinary actions.
Re-credentialing
- Healthcare providers who are already part of an organization or network are periodically re-evaluated and verified for their credentials.
- This typically occurs every three years, but the frequency can vary depending on organizational policies or state regulatory requirements.
- Re-credentialing involves re-evaluating a provider’s competence, performance, and compliance with current healthcare standards.
Provisional Credentialing
- Providers with provisional credentials are granted this status in order to expedite the process of providing care, often during the processing of a full credentialing application.
- This process involves a preliminary review of the provider’s qualifications to ensure they meet minimum standards.
- A provisional credentialing process is time-limited, with the expectation that the full credentialing process will take place within a certain amount of time.
Need Help with Credentialing in Medical Billing?
Do you need help with credentialing? Don’t worry, 360Connect has got your back! Just fill out our 1-2 minute form and then we will call you to verify your information and needs. From there, up to 5 suppliers will reach out with quotes for services for medical credentialing. This process is 100% free and easy to use!

